What is this drug used for?
GLP-1 injection is a human GLP-1 analog; and selectively binds to and activates the GLP-1 receptor. GLP-1 is a physiological regulator of appetite and caloric intake and is present in several areas of the brain involved with appetite regulation.
GLP-1 injection stimulates insulin secretion and reduces glucagon secretion in a glucose dependent manner, which can lead to a reduction of blood glucose.
What do I need to tell my doctor BEFORE I take this drug?
- If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances.
- Tell your doctor about the allergy and what signs you had.
- If you have type 1 diabetes. Do not use this drug to treat type 1 diabetes.
- If you have ever had pancreatitis.
- If you have stomach or bowel problems.
- This is not a list of all drugs or health problems that interact with this drug.
- This is not a list of all drugs or health problems that interact with this drug.
What are some things I need to know or do while I take this drug?
- Tell all of your health care providers that you take this drug. This includes your doctors, nurses, pharmacists, and dentists.
- Follow the diet and workout plan that your Lindora Provider told you about.
- Birth control pills may not work as well to prevent pregnancy. If you take birth control pills, you may need to switch to another type of hormone-based birth control like a vaginal ring if your doctor tells you to. If another type of hormone-based birth control is not an option, use some other kind of birth control also, like a condom. Do this for 4 weeks after starting this drug and for 4 weeks each time the dose is raised.
- This drug may prevent other drugs taken by mouth from getting into the body. If you take other drugs by mouth, you may need to take them at some other time than this drug. Talk to your doctor.
- Talk with your doctor before you drink alcohol.
- If you cannot drink liquids by mouth or if you have upset stomach, throwing up, or diarrhea that does not go away; you need to avoid getting dehydrated. Contact your Lindora Provider to find out what to do. Dehydration may lead to new or worse kidney problems.
- A severe and sometimes deadly pancreas problem (pancreatitis) has happened with other drugs like this one.
- Tell your doctor if you are pregnant, plan to try to become pregnant, or are breast-feeding. You will need to talk about the benefits and risks with your doctor to you and the baby.
What are some things I need to know or do while I take this drug?
Warning/Caution:
Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
- Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
- Signs of kidney problems like unable to pass urine, change in how much urine is passed, blood in the urine, or a big weight gain.
- Signs of gallbladder problems like pain in the upper right belly area, right shoulder area, or between the shoulder blades; yellow skin or eyes; fever with chills; bloating; or very upset stomach or throwing up.
- Signs of a pancreas problem (pancreatitis) like very bad stomach pain, very bad back pain, or very bad upset stomach or throwing up.
- Dizziness or passing out.
- A fast heartbeat.
- Change in eyesight.
- Low blood sugar can happen. The chance may be raised when this drug is used with other drugs for diabetes. Signs may be dizziness, headache, feeling sleepy or weak, shaking, fast heartbeat, confusion, hunger, or sweating. Call your doctor right away if you have any of these signs. Follow what you have been told to do for low blood sugar. This may include taking glucose tablets, liquid glucose, or some fruit juices.
Warnings
This drug has been shown to cause thyroid cancer in some animals. It is not known if this happens in humans. If thyroid cancer happens, it may be deadly if not found and treated early. Call your doctor right away if you have a neck mass, trouble breathing, trouble swallowing, or have hoarseness that will not go away. Have your blood work checked and thyroid ultrasounds as you have been told by your doctor.
Do not use this drug if you have a health problem called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2), or if you or a family member have had thyroid cancer
What are some other side effects of this drug?
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
- Constipation, diarrhea, stomach pain, upset stomach, throwing up, or decreased appetite.
- Heartburn.
These are not all of the side effects that may occur. If you have questions about side effects, call your Lindora Provider. Call your Lindora Provider for medical advice about side effects.
You may report side effects to your national health agency.
How is this drug best taken?
- Use this drug as ordered by your Lindora Provider. Read all the information given to you. Follow all instructions closely.
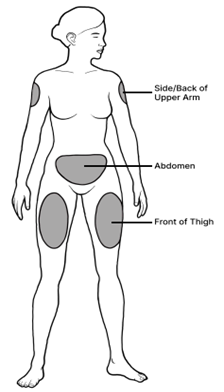
- It is given as a shot into the fatty part of the skin on the top of the thigh, belly area, or upper arm.
- If you will be giving yourself the shot, your Lindora nurse will teach you how to give the shot.
- Keep taking this drug as you have been told by your Lindora Provider.
- Take the same day each week.
- Move site where you give the shot each time.
- Take with or without food.
- Wash your hands before and after use.
- Do not use if the solution is leaking or has particles.
- This drug is colorless to a faint yellow. Do not use if the solution changes color.
- Throw away needles in a needle/sharp disposal box. Do not reuse needles or other items. When the box is full, follow all local rules for getting rid of it. Talk with a Lindora Provider or pharmacist if you have any questions.
What do I do if I miss a dose?
- If it is within 4 days after the missed dose, take the missed dose and go back to your normal day.
- If it has been more than 4 days since the missed dose, skip the missed dose and go back to your normal day.
- If one (1) week is missed, the patient will resume with the titration schedule for the upcoming weeks, as long as the patient is tolerating potential side effects of the increased dose.
- If two (2) weeks are missed, the patient will need to restart the titration from week 1.
- Do not take 2 doses at the same time or extra doses.
How do I store and/or throw out this drug?
- Store in a refrigerator. Do not freeze.
- Do not use if it has been frozen.
- After puncturing the vial, throw away any remaining medication not used after 28 days.
- Protect from heat.
- Store in the original container to protect from light.
- Keep all drugs in a safe place. Keep all drugs out of the reach of children and pets.
- Throw away unused or expired drugs. Do not flush down a toilet or pour down a drain unless you are told to do so. Check with your pharmacist if you have questions about the best way to throw out drugs. There may be drug take-back programs in your area.
General drug facts
- If your symptoms or health problems do not get better or if they become worse, call your doctor.
- Do not share your drugs with others and do not take anyone else’s drugs.
- Some drugs may have another patient information leaflet. If you have any questions about this drug, please talk with your doctor, nurse, pharmacist, or other health care provider.
- If you think there has been an overdose, call your poison control center or get medical care right away. Be ready to tell or show what was taken, how much, and when it happened.
Instructions for Self-Administration of Medication
Drawing your medication
Step 1. Check the medication label. Make sure your medication matches the dosage prescribed by your provider.
Step 2. Remove the lid from your vial.
Step 3. With the syringe cap still on, pull back the plunger to the 50 mark (0.5ml) on your syringe. This fills the syringe with air.

Step 4. Remove the syringe cap and insert the needle into the rubber top and push all of the air into the vial.
Step 5. Turn the vial upside down and pull the plunger back to the 50 mark again to draw 0.5ml of medication.
Step 6. If you see air bubbles in the syringe, keep the tip inserted and tap the syringe with your finger until the bubbles move to the top. Then gently push the plunger to push the air bubbles back into the vial.

Injecting your medication
Step 1. Remember to rotate your injection site. You should be at least 1 ½ inches away from the last injection site.
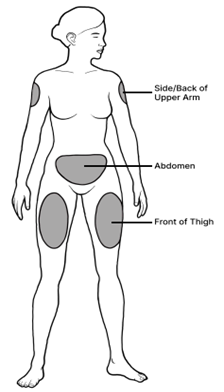
Step 2. Select your injection site and cleanse the area with an alcohol wipe. Wait for the site to dry.
Step 3. Pinch a 2-inch fold of skin between your thumb and index finger.
Step 4. Hold the Syringe the way you would a pencil or dart. Insert the needle at a 45-to-90-degree angle to the pinched-up skin. The needle should be completely covered by skin.
Step 5. Hold the syringe with one hand. With the other, pull back the plunger to check for blood. If you see blood in the solution in the syringe, do not inject. Withdraw the needle and start again at a new site. If you do not see blood, slowly push the plunger to inject the medication. Press the plunger all the way down.
Step 6. Remove the needle from the skin and gently hold an alcohol pad on the injection site. Do not rub.
Consumer Information Use and Disclaimer
This generalized information is a limited summary of diagnosis, treatment, and/or medication information. It is not meant to be comprehensive and should be used as a tool to help the user understand and/or assess potential diagnostic and treatment options. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider’s examination and assessment of a patient’s specific and unique circumstances. Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications. This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient.
